Fistula
A fistula is an abnormal passageway that connects two organs or tissues that do not usually connect. It can develop anywhere in the body due to infection, injury, inflammation, or surgery.
Causes of Fistula
Fistulas can form due to:
- Infections – Chronic infections can create an abscess, which may erode tissues and form a fistula.
- Inflammatory conditions – Diseases like Crohn’s disease and ulcerative colitis increase the risk.
- Surgery or trauma – Post-surgical complications or injuries may cause fistula formation.
- Obstruction – Blockages in ducts or organs can lead to pressure buildup and fistula development.
- Radiation therapy – Damage from radiation treatment can lead to fistula formation.
- Cancer – Tumors can erode tissues, creating a fistula.
Types of Fistulas
Digestive Fistulas
These involve the gastrointestinal (GI) tract and may cause leakage of fluids or waste into other areas.
- Enterocutaneous fistula (ECF) – Between the intestine and skin.
- Colovesical fistula – Between the colon and bladder, leading to urinary tract infections (UTIs).
- Enteroenteric fistula – Between different parts of the intestine.
- Gastrocutaneous fistula – Between the stomach and skin.
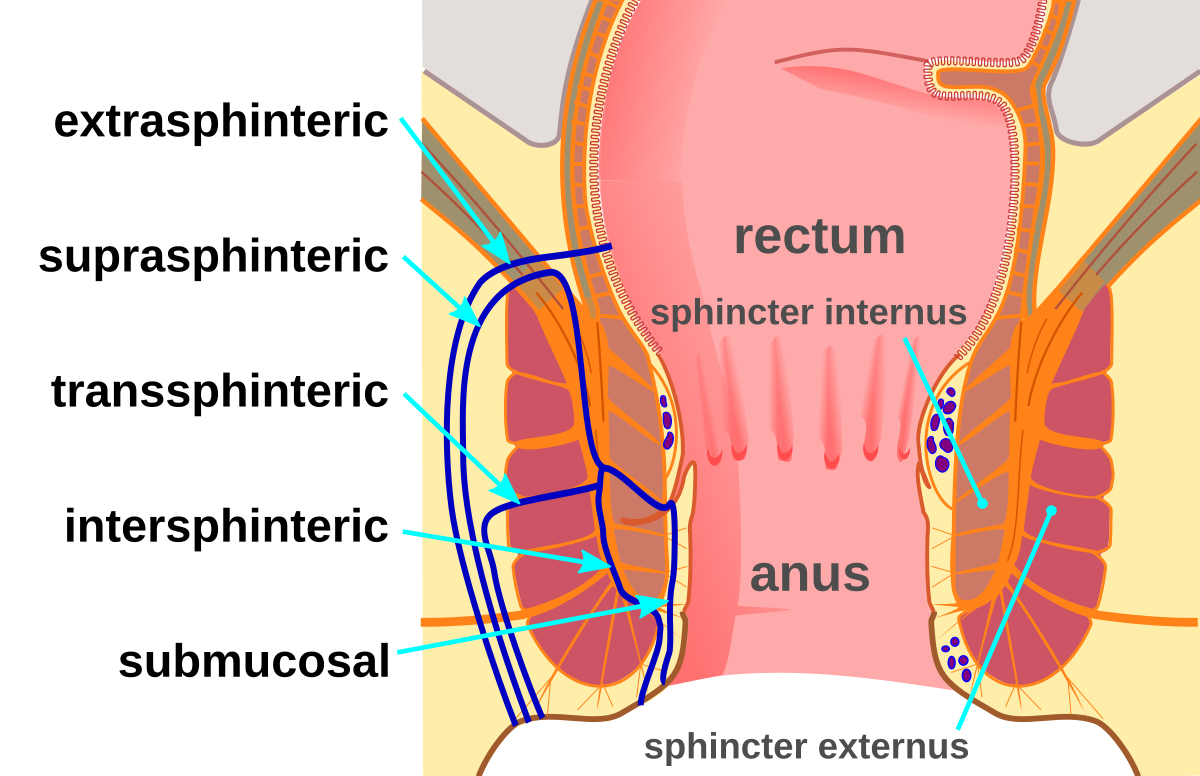
Anal Fistula
- Forms between the anal canal and the skin near the anus, often due to an abscess.
- Common in people with Crohn’s disease or after an anal infection.
- Symptoms: Pain, swelling, pus or stool drainage, redness around the anus.
Urinary Fistulas
- Vesicovaginal fistula – Between the bladder and vagina, leading to urine leakage from the vagina.
- Urethral fistula – Between the urethra and skin, often due to trauma or surgery.
- Ureteral fistula – Between the ureter and another organ, usually caused by surgery or kidney stones.
Obstetric Fistula
- Occurs due to prolonged, obstructed labor, leading to a connection between the vagina and bladder (vesicovaginal) or rectum (rectovaginal).
- Common in areas with limited access to maternal healthcare.
Arteriovenous Fistula (AVF)
- Abnormal connection between an artery and a vein.
- Can be congenital, occur due to trauma, or be surgically created for dialysis in kidney failure patients.
Symptoms of Fistulas
Symptoms vary depending on the type and location but may include:
- Chronic drainage of pus, feces, or urine from an abnormal opening.
- Pain and swelling.
- Recurrent infections.
- Fever (if infected).
- Skin irritation around the fistula site.
- Incontinence (loss of control over urine or stool).
Diagnosis of Fistula
1. Physical Examination
- For external fistulas (e.g., anal fistulas), a doctor may visually inspect the affected area.
2. Imaging Tests
- CT Scan/MRI – Helps identify internal fistulas and assess complications.
- Fistulography – A contrast dye is injected to visualize the fistula path.
- Ultrasound – Used for detecting soft tissue fistulas.
- X-ray with Contrast – Helps identify gastrointestinal or urinary fistulas.
3. Endoscopy/Colonoscopy
- Used to examine fistulas inside the digestive tract or urinary system.
4. Laboratory Tests
- Blood tests may show signs of infection or inflammation.
Treatment of Fistula
1. Medications
- Antibiotics – Used if the fistula is infected.
- Anti-inflammatory drugs – For Crohn’s-related fistulas.
- Immunosuppressants – Help reduce inflammation in conditions like Crohn’s disease.
2. Surgery
- Fistulotomy – The fistula is cut open to heal from the inside out (used for anal fistulas).
- Fistula repair/reconstruction – Tissue grafts or flaps may be used to close large fistulas.
- Seton Placement – A small surgical thread is placed to keep the fistula open for drainage.
- Stoma surgery – In severe cases, an artificial opening (stoma) is created for waste removal.
3. Fistula Plugs
- Biodegradable materials (such as collagen plugs) are used to block and help the fistula heal.
4. Drainage
- If a fistula is associated with an abscess, it may need to be drained before further treatment.
5. Catheter or Stent Placement
- In urinary or gastrointestinal fistulas, a catheter or stent may be used to allow healing.
Complications of Fistulas
- Infections (sepsis) – If untreated, infections can spread.
- Malnutrition – Digestive fistulas may lead to nutrient loss.
- Skin irritation and ulcers – Due to continuous leakage.
- Incontinence – In cases of anal or rectovaginal fistulas.
Prevention of Fistulas
- Early treatment of infections and abscesses.
- Managing conditions like Crohn’s disease properly.
- Good surgical care to avoid post-operative fistulas.
- Proper maternal healthcare to prevent obstetric fistulas.
