Piles / Hemorrhoids
Hemorrhoids (or piles) are swollen vascular structures (varicose veins) in the anal canal. In their normal state, these cushions help with stool control. They become a problem when they become enlarged, inflamed, or prolapsed.
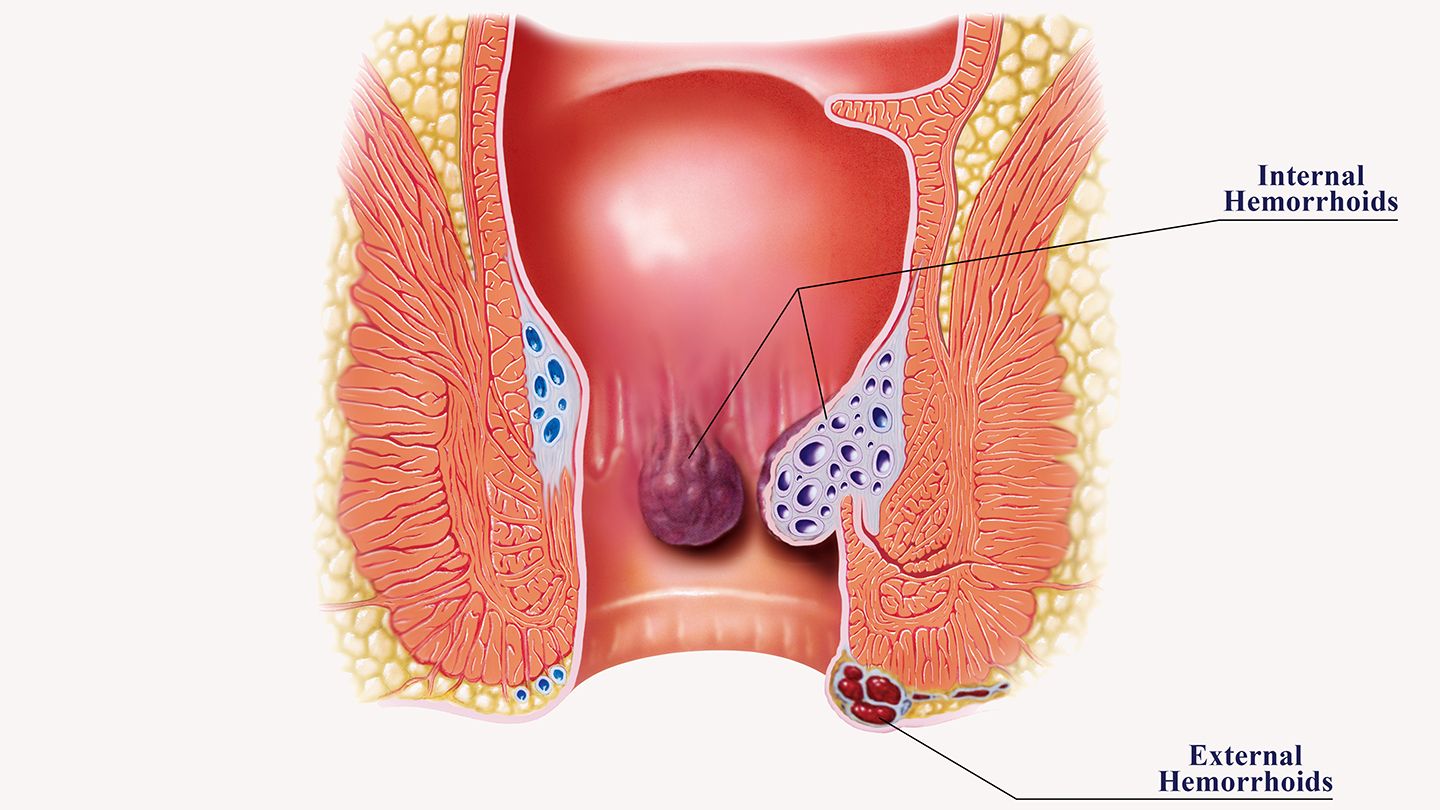
Types:
Internal Hemorrhoids:
- Occur inside the rectum above the pectinate (dentate) line.
- Typically painless because this area lacks pain receptors.
- Common symptom: Painless, bright red rectal bleeding during or after bowel movements.
Graded as:
- Grade I: Bleeding only, no prolapse
- Grade II: Prolapse during defecation but self-reduces
- Grade III: Prolapse requiring manual reduction
- Grade IV: Prolapsed and irreducible
- External Hemorrhoids: Occur under the skin around the anus (below the pectinate line).
- Can be painful and itchy because the skin is richly innervated.
- If a blood clot forms (thrombosed hemorrhoid), it causes severe pain and swelling.
Prolapsed Hemorrhoids:
- Internal hemorrhoids that have descended and are visible externally.
- May cause discomfort and require manual reduction.
Causes and Risk Factors
Main Factors: Although the precise cause is not fully understood, several factors are believed to contribute:
Increased Intra-abdominal Pressure:
- Chronic constipation or diarrhea leading to straining during bowel movements
- Prolonged sitting on the toilet
- Heavy lifting
Pregnancy:
- The pressure of the growing uterus and hormonal changes can enlarge hemorrhoidal vessels.
Diet:
- A low-fiber diet can lead to hard stools and straining.
- Aging and Genetic Predisposition:
- Tissues may weaken with age and hereditary factors might predispose some individuals.
Non-surgical Procedures:
Rubber Band Ligation:
- An elastic band is placed around an internal hemorrhoid to cut off its blood supply, causing it to shrink and fall off.
Sclerotherapy:
- Injection of a sclerosing agent (like phenol) into the hemorrhoid to induce fibrosis and shrinkage.
Infrared Photocoagulation:
- Infrared light is used to coagulate and shrink small hemorrhoids.
Electrocoagulation:
- A small electric current creates scar tissue to reduce blood flow.
Surgical Options:
Hemorrhoidectomy:
- Surgical removal is considered for severe or recurrent cases (especially Grade III–IV or thrombosed external hemorrhoids).
- Though effective, it is associated with significant postoperative pain and longer recovery.
Stapled Hemorrhoidopexy:
- A stapling device repositions prolapsed hemorrhoids and cuts off their blood supply.
- Usually less painful with a quicker recovery but may have higher recurrence rates.
Doppler-guided Hemorrhoidal Artery Ligation (DGHAL):
- A minimally invasive procedure that uses Doppler ultrasound to locate and ligate the hemorrhoidal arteries.
Pathophysiology
In healthy individuals, hemorrhoid cushions help with continence by contributing to the closure pressure of the anus. When these cushions become engorged or slide downward (due to weakening of supporting tissues), they manifest as symptomatic hemorrhoids. Abnormal dilatation, inflammation, thrombosis, or prolapse of these vascular structures underlies the condition.
Symptoms
Internal Hemorrhoids:
- Painless bright red bleeding during bowel movements
- Possible prolapse leading to a visible bulge
External Hemorrhoids:
- Pain, especially if thrombosed
- Itching, swelling, and discomfort around the anus
- A lump or skin tag after healing
Other symptoms may include a feeling of incomplete evacuation, mucous discharge, and, in rare cases, discomfort severe enough to affect daily activities.
Diagnosis
Diagnosis typically involves:
Physical Examination:
- Visual inspection of the anus for external hemorrhoids
- Digital rectal exam to assess internal structures
Anoscopy or Proctoscopy:
- Used to visualize internal hemorrhoids if they are not palpable.
Colonoscopy or Sigmoidoscopy:
- Recommended if bleeding is significant or to rule out other causes (such as colorectal cancer).
Treatment Options
Conservative Measures:
Diet and Lifestyle:
- Increase fiber intake (via diet or supplements) to soften stools and reduce straining
- Stay well-hydrated
- Regular exercise and weight management
Home Remedies:
- Warm sitz baths
- Topical treatments (creams or suppositories containing witch hazel, hydrocortisone, or lidocaine) for temporary relief
- Over-the-counter pain relievers (NSAIDs)
Prevention
To help prevent hemorrhoids:
- Eat a high-fiber diet rich in fruits, vegetables, and whole grains.
- Drink plenty of fluids to keep stools soft.
- Avoid prolonged straining and sitting on the toilet.
- Exercise regularly and maintain a healthy weight.
- Avoid heavy lifting and address chronic constipation or diarrhea promptly.
Additional Considerations
When to Seek Medical Attention:
- Persistent bleeding or severe pain
- Signs of infection (fever, pus)
- Symptoms that do not improve with home treatment
